In modern medicine, the thought of performing surgery without wearing gloves is utterly unthinkable. It is common knowledge that their use helps to prevent the transmission of infection in operating theatres, as well as protecting the surgeon and other staff. This was, however, not always the case, and before the late 1800s, no surgeon wore gloves.
The introduction of the surgical glove in 1889 had a massive impact on the safety of surgery and would save countless lives. Few people realise that the reason they were introduced has its roots in a love story.
A (Very) Brief History of Rubber
It is important to state that without the discovery of rubber, we would also not have surgical gloves today. Before we move on to the romantic aspect of this article, let’s go back in time to 1500 BCE. The earliest evidence of the use of natural latex comes from the ancient Mesoamerican Olmec culture, the oldest known major civilisation in the Mexico region. At this time it was apparently used for making balls for a game that is not entirely dissimilar to racquetball.
The Frenchman Charles Marie de La Condamine is credited with the introduction of rubber samples to Europe in 1736, and in 1770 the Englishman Joseph Priestly observed that it was particularly good at rubbing off pencil marks from paper, hence the name “rubber.”
The first rubber processing procedure, vulcanisation, was developed by Charles Goodyear in 1839. He treated crude rubber with sulphur and subjected it to heat. This process made the rubber less plastic and increased its strength and durability. Following this, the use of rubber became increasingly popular, and in the 1870s the commercial cultivation of rubber was introduced by British planters in India, at the Calcutta Botanical Gardens. By the latter part of the 19th-century rubber was widely available and was being used for an increasingly diverse number of commercial and industrial uses.
Joseph Lister and Surgical Asepsis
In the late 1890s surgery still had a 50% mortality rate and infection caused the majority of these deaths. Most of these deaths were preventable as surgeons did not wash hands between procedures or carry out even the most basic of hygiene practices.
This would all change with the introduction of the use of carbolic acid to sterilise surgical instruments by Joseph Lister. Lister initially used the carbolic acid to clean compound fracture wounds, and the results were quite remarkable, reducing mortality rates dramatically. Spurred on by the success of his early experiments, Lister developed a machine that distributed a fine mist of carbolic acid into the operating theatre around the surgical site. The surgical instruments were also washed in the same solution. The combination of these antiseptic measures resulted in a dramatic fall in the death rate of Lister’s surgical patients from close to 50% to only 15% in 1870.
The introduction of the use of carbolic acid would also be indirectly responsible for the development of surgical gloves through a sequence of chance events.
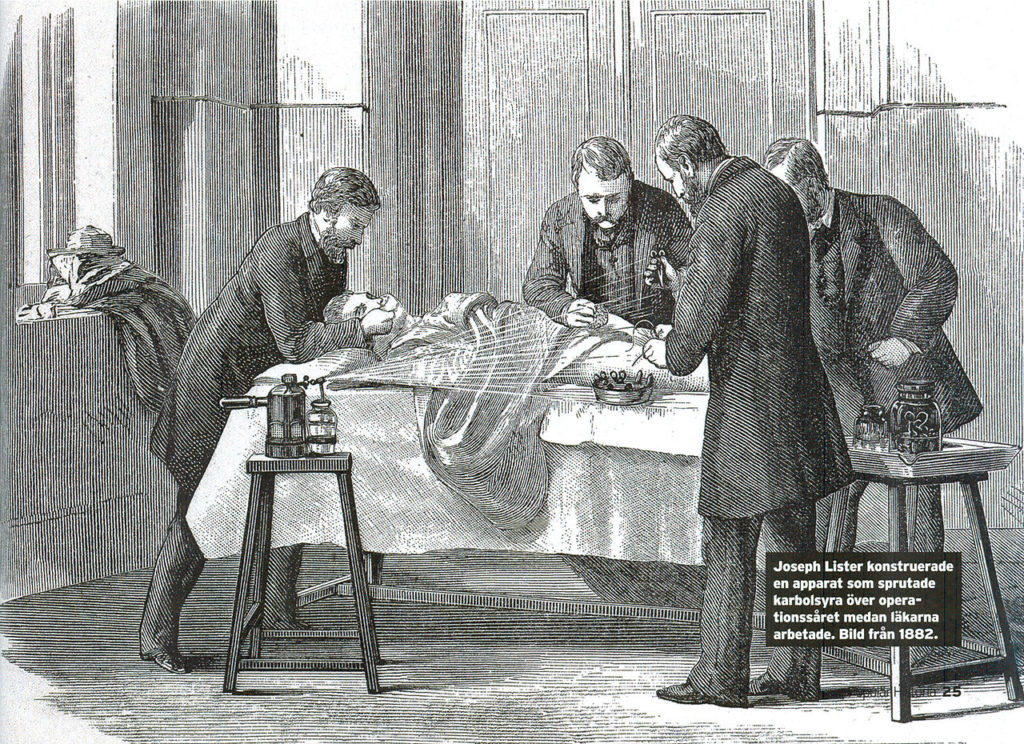
Joseph Lister spraying a patient with carbolic acid during a surgical procedure.
William Halsted and Caroline Hampton
William Stewart Halsted was one of the “Big Four” founding professors of the Johns Hopkins Hospital. He was responsible for the development and introduction of several important surgical procedures, including radical mastectomy for breast cancer, as well as the establishment of the first training program and residency system for young surgeons.
Caroline Hampton was a member of a prominent American southern family and the niece of Confederate General Wade Hampton III. She rebelled against her family wishes and entered nursing school in New York City, graduating in 1888. In 1889 she moved to Baltimore, and it was here the two would meet, and the love story would begin. She was appointed chief nurse to William Halsted, and before long the two would become romantically involved.
Following the work by Lister, Halsted decided to use a combination of carbolic acid and mercuric chloride as a disinfectant during his surgical procedures. Hampton, acting as his scrub nurse would have to handle these chemicals regularly, and as a consequence, she developed severe contact dermatitis on her hands. Halsted could not bear to see her go through this and reached out to the Goodyear Rubber Company to create a rubber glove that she could wear during surgery to protect her hands. Halsted explains, (as quoted by Sherwin Nuland in ‘Doctors: The Biography of Medicine’):
“In the winter of 1889 and 1890, I cannot recall the month, the nurse in charge of my operating-room complained that the solutions of mercuric chloride produced a dermatitis of her arms and hands. As she was an unusually efficient woman, I gave the matter my consideration and one day in New York requested the Goodyear Rubber Company to make as an experiment two pair of thin rubber gloves with gauntlets. On trial these proved to be so satisfactory that additional gloves were ordered. In the autumn, on my return to town, an assistant who passed the instruments and threaded the needles was also provided with rubber gloves to wear at the operations. At first the operator wore them only when exploratory incisions into joints were made. After a time the assistants became so accustomed to working in gloves that they also wore them as operators and would remark that they seemed to be less expert with the bare hands than with the gloved hands.”
The two were married in June of 1890, shortly after he presented her with two pairs of rubber gloves made to fit plaster casts of her hands. Before long other theatre staff and surgeons began wearing the gloves too, and in time their use became commonplace. At this time the gloves were only used to protect the hands of the staff, but in 1894 Lister became the first person to sterilise the rubber gloves used in surgery.
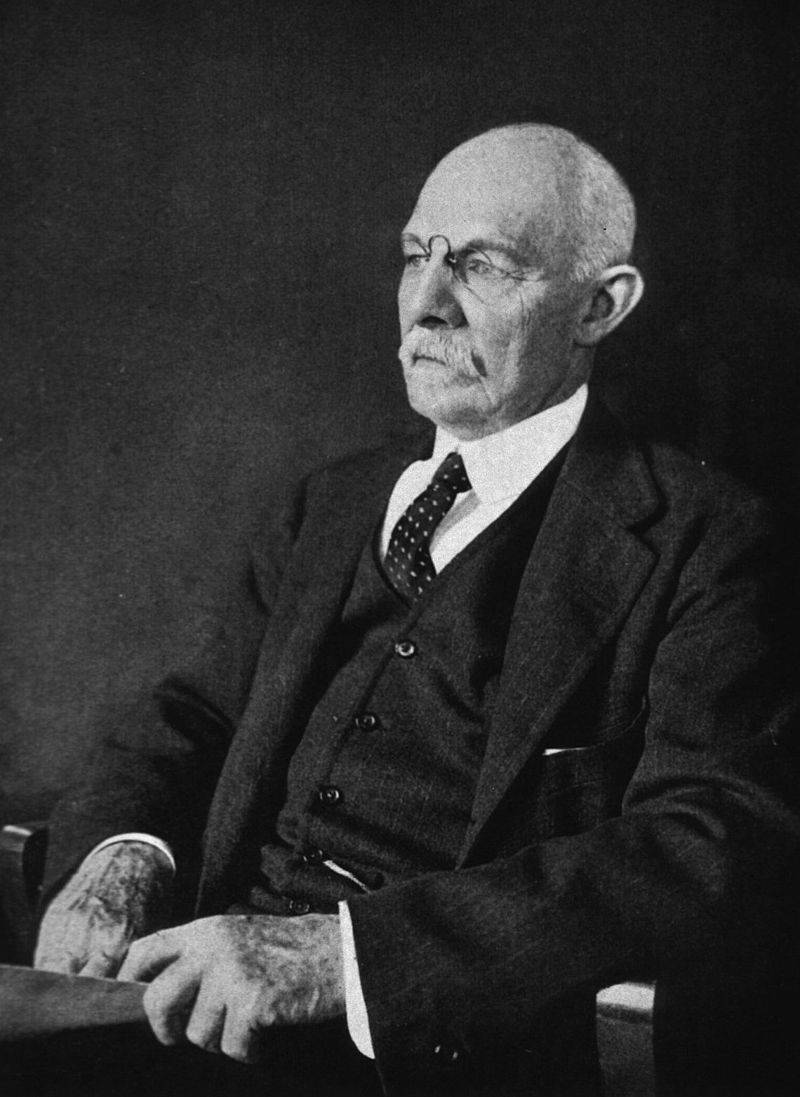
William Halsted, pictured in 1922
The Evolution of the Modern Surgical Glove
By the early 1900s, all surgeons were wearing sterile rubber gloves. The first disposable latex medical gloves were manufactured in 1964 by the Ansell Rubber company. These gloves were sterile sterilised the gloves using gamma irradiation and were then disposed of following surgery. Disposable surgical gloves are now the standard in the operating room and many surgeons ‘double glove’ when performing procedures to reduce the danger of infection from glove failure or puncture.
Talcum powder was introduced to make the donning of gloves easier, but over recent years evidence has arisen that this is linked to the development of post-operative scars and inflammation. In December 2016, the use of powdered gloves was banned.
Another recent development is the introduction of non-latex gloves. The constant wearing of latex gloves has led to an increasing rate of latex allergy in both medical professionals and patients, and gloves made of non-latex materials, such as polyvinyl chloride and neoprene have become widely used.




Really enjoyed the History of Surgical Gloves. Thank you!